This article is for informational purposes only and should not be considered medical advice. Always consult a healthcare professional for personalized guidance.
Understanding Diabetes Symptoms
Diabetes is a chronic condition that affects how your body metabolizes sugar (glucose), a vital source of energy for your body. Managing diabetes symptoms effectively can significantly enhance your quality of life. Symptoms may vary depending on the type of diabetes—Type 1 or Type 2—but common signs include increased thirst, frequent urination, fatigue, and blurred vision.
Recognizing the Signs
It’s crucial to recognize these symptoms early. For instance, if you find yourself drinking more water than usual or needing to urinate frequently, it might be time to check your blood sugar levels. The American Diabetes Association suggests keeping a close eye on these indicators, especially if you have a family history of diabetes.
Pathophysiology of Diabetes
Understanding the underlying mechanisms of diabetes can empower you in managing the condition. In Type 1 diabetes, the immune system mistakenly attacks insulin-producing beta cells in the pancreas, leading to little or no insulin production. Conversely, Type 2 diabetes is characterized by insulin resistance, where the body’s cells do not respond effectively to insulin, often coupled with an eventual decline in insulin production. This dual pathology results in elevated blood glucose levels, which can lead to complications if not managed properly.
Moreover, chronic hyperglycemia can create a vicious cycle. High blood sugar levels can damage blood vessels, leading to complications such as neuropathy, retinopathy, and cardiovascular diseases. Understanding these mechanisms can motivate individuals to adhere to their management plans more rigorously.
Effective Strategies for Managing Symptoms
Managing diabetes symptoms involves a multi-faceted approach that includes lifestyle changes, dietary adjustments, and medication adherence. Here are several effective strategies:
1. Monitor Your Blood Sugar Levels
Regularly checking your blood glucose levels is essential. This practice helps you understand how different foods, activities, and medications affect your blood sugar. The CDC recommends aiming for a target range of 80-130 mg/dL before meals and less than 180 mg/dL two hours after meals. Consider using continuous glucose monitors (CGMs) for real-time data, which can provide insights into your glucose trends.
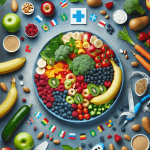
2. Adopt a Balanced Diet
Your diet plays a pivotal role in managing diabetes. Focus on consuming whole foods rich in fiber, such as vegetables, fruits, whole grains, and legumes. For instance, a meal of quinoa salad with mixed greens and grilled chicken can provide essential nutrients while keeping your blood sugar stable. It’s also beneficial to be mindful of portion sizes and meal timing, as these can impact blood sugar levels.
Carbohydrate Counting
Understanding carbohydrate intake is critical. Carbohydrates affect blood sugar levels more than other macronutrients. Consider using apps or tools to help you track your carb intake effectively. Aim to distribute your carbohydrate intake evenly throughout the day to avoid spikes in blood sugar.
3. Engage in Regular Physical Activity
Exercise helps lower blood sugar levels and improves insulin sensitivity. Aim for at least 150 minutes of moderate aerobic activity each week, such as brisk walking or cycling. Incorporating strength training exercises at least twice a week can also be beneficial. For example, a simple routine of bodyweight exercises like squats and push-ups can enhance muscle mass, which plays a crucial role in glucose metabolism.
4. Medication Management
If prescribed, take your medications as directed. Insulin therapy may be necessary for some individuals with Type 1 diabetes or advanced Type 2 diabetes. Always consult your healthcare provider for adjustments based on your blood sugar readings. Additionally, familiarize yourself with the different classes of diabetes medications, such as metformin or GLP-1 receptor agonists, to understand their mechanisms and potential side effects.
5. Stay Hydrated
Proper hydration is often overlooked. Drinking enough water helps your kidneys flush out excess sugar through urine. Aim for at least eight 8-ounce glasses of water daily, adjusting based on activity level and climate. Dehydration can lead to higher blood sugar levels, so keep a water bottle handy to encourage regular intake.
6. Manage Stress
Stress can impact your blood sugar levels. Techniques such as mindfulness, yoga, and meditation can help reduce stress. Consider dedicating time each day to activities that promote relaxation. For instance, practicing deep breathing exercises for just a few minutes can lower cortisol levels, which in turn can help stabilize blood sugar.
Patient Vignette
Meet Sarah, a 45-year-old woman diagnosed with Type 2 diabetes. Initially overwhelmed by her diagnosis, she began monitoring her blood sugar levels diligently. With the help of a nutritionist, she adopted a balanced diet, incorporating more whole foods and reducing sugary snacks. Sarah also joined a local walking group, which not only improved her fitness but also provided a supportive community. Within months, she noticed a significant reduction in her symptoms and felt empowered to manage her condition. Sarah’s journey illustrates that with the right strategies and support, it is possible to take control of diabetes.
Common Myths vs. Facts
| Myth | Fact |
|---|---|
| People with diabetes can’t eat sugar. | Moderation is key; people with diabetes can enjoy sweets occasionally as part of a balanced diet. |
| Diabetes is not a serious condition. | Diabetes can lead to severe complications, including heart disease, kidney failure, and vision loss if not managed properly. |
| Only overweight people get diabetes. | While obesity is a risk factor, diabetes can affect individuals of all body types. |
| Insulin is a cure for diabetes. | Insulin is a treatment, not a cure. It helps manage blood sugar levels but does not eliminate the disease. |
| Once you have diabetes, you can’t go back to normal. | With lifestyle changes, some individuals can achieve remission, particularly in Type 2 diabetes. |
FAQs About Managing Diabetes Symptoms
What should I eat to manage diabetes?
Focus on a diet rich in vegetables, whole grains, lean proteins, and healthy fats. Limit processed foods and sugars. Incorporate foods with a low glycemic index to help maintain stable blood sugar levels.
How often should I check my blood sugar?
Consult your healthcare provider for personalized recommendations, but generally, checking before and after meals can be beneficial. Continuous monitoring may be necessary for those on insulin.
Can exercise help lower blood sugar?
Yes, regular physical activity can improve insulin sensitivity and lower blood sugar levels. Activities like walking, swimming, or cycling can be effective.
What are the signs of low blood sugar?
Symptoms include shakiness, sweating, confusion, and irritability. It’s important to treat low blood sugar promptly by consuming fast-acting carbohydrates, such as glucose tablets or juice.
How can I manage stress related to diabetes?
Engage in stress-reducing activities such as yoga, meditation, or talking to a therapist. Building a support network can also help alleviate feelings of isolation.
Is it possible to reverse Type 2 diabetes?
While there is no cure, many individuals can achieve remission through lifestyle changes, weight loss, and medication adherence. Regular follow-ups with your healthcare provider are essential to monitor progress.
What are some practical tips for managing diabetes?
Consider meal prepping to avoid unhealthy choices when you’re busy. Keep healthy snacks on hand, like nuts or yogurt, to maintain stable blood sugar levels between meals. Additionally, setting reminders for medication and hydration can be beneficial.
Can stress really affect my blood sugar levels?
Absolutely. Stress triggers the release of hormones like cortisol, which can raise blood sugar levels. Finding effective stress management techniques is crucial for maintaining your overall health.
Key Takeaways
- Regularly monitor your blood sugar levels to understand how your body responds to food and activity.
- Adopt a balanced diet rich in whole foods and low in processed sugars.
- Incorporate regular physical activity to improve insulin sensitivity.
- Manage stress through mindfulness and relaxation techniques.
- Stay hydrated to help your kidneys manage excess sugar.
- Adhere to medication plans as prescribed by your healthcare provider.
References
- American Diabetes Association. Standards of Medical Care in Diabetes—2023.
- Centers for Disease Control and Prevention. Diabetes Basics.
- National Health Service. Diabetes: Symptoms and Complications.
- PubMed Central. Lifestyle Interventions for Diabetes Management.
- World Health Organization. Diabetes Fact Sheet.
- UpToDate. Management of Type 2 Diabetes Mellitus in Adults.



Post a comment